MOREL-LAVALLEE LESION: case report and literature review on diagnosis and management of post-traumatic MLL in polytrauma patients.
Introduction.
Morel-Lavallee lesion has become an eponym since Maurice Morel-Lavallee described the first closed degloving injury in 1853. In present days, Morel-Lavallee lesion is still a rare condition resulting from blunt shearing of soft tissues due to trauma that separates the hypodermis from underlying fascia. The cavity that is created between the separated skin with subcutaneous tissue and fascia becomes filled with blood due to injury to perforating arteries as well as necrotic tissues. Although the MLL is often seen in traumatic injuries to lower extremities, mostly secondary to MVCs, however, they are also seen on trunk and buttocks.
The closed cavity formed between subcutaneous tissue and fascia may remain unrecognized for some time. However, often the lesion is easily identified on CT or MRI as well as US images taken as part of complex work up of trauma patient or for soft tissue swelling in patient with history of blunt trauma. With time the closed cavity becomes organized secondary to inflammatory reaction and subsequent development of granulation tissue and the fibrous pseudocapsule. And as the pseudocapsule is formed around the contents of the MLL, patients often have no specific clinical symptoms, except for swelling of the site. The contents of the MLL thus may remain unrecognized for many days or even months.

Photo: Large Morel-Lavalee lesion of the anterior thigh.

Photo: MRI of the patient who sustained the traumatic injury resulted in Large Morel-Lavalee lesion of the right hip.
The diagnosis of MLL although may present a challenge, however, is important. The closed cavity of the MLL often gets infected due to presence of necrotic tissues and hematoma. The physical examination is an important element of diagnostic work up for MLL along with diagnostic imaging. The soft tissue swelling at the site of blunt trauma is an important clue to the further evaluation of patient for MLL. Often the fluctuation or hypermobility of the skin can be observed during examination, but this may appear several days after the traumatic insult.
Although almost all trauma patients initially get plain Xray films for evaluation of acute pathologies of chest, abdomen and pelvis, these films would only show soft tissue swelling. In acute setting of severe trauma when most patients get CT imaging, the MLL of buttocks, lumbodorsal region and greater trochanter can be easily diagnosed. The use of US imaging for diagnosis of MLL has been reported in several case series. US diagnosis of MLL is based on identification of anechoic areas between hypodermis and fascial planes. MRI has also been reported to be useful in diagnosis of MLL. In the report by Mellado et al (1997) the MRI diagnosis of MLL was made by observation of fusiform or oval shaped mass with well-defined borders and containing in the deep subcutaneous space. The demonstration of the capsule on imaging can be very useful in making a decision towards the conservative vs. aggressive surgical treatment. The MRI and US are even more helpful in diagnostic work up of small size MLL without pseudocapsule as these lesions, particularly in children or young patients, may mimic the soft tissue tumors.
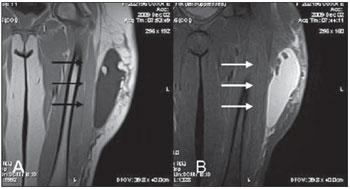
Photo: MRI of the left thigh with large Morel-Lavalee lesion in the patient who sustained the car accident.
Brief literature review.
MLL are often associated with the pelvic ring fractures and greater trochanter fractures. According to S.A. Kottmeier et al (1996) and D.J. Hak et al (1997) there is a high likelihood of acetabular and pelvic fractures associated with MLL.
There is no unified approach to the treatment of MLL. Some experts consider surgical treatment as better than conservative approach consisting of drainage and pressure dressing or sclerosotherapy. Letournel and Judet (1993) used the term Morel-Lavallee lesion for the first time to describe the closed soft tissue degloving injury and also suggested that these lesions shall be aspirated or decompressed as soon as they are recognized. Hudson D.A. et al (1992) suggested the evacuation of hematoma and necrotic tissue through small incision over the lesion and placement of the drain. Since the work of Letournel and Judet (1993) number of methods have been proposed for the treatment of MLL, including aspiration, incision and drainage with placement of drain through normal skin, wide surgical excision and compression dressings.
Hak D.J. et al (1997) described 24 patients with MLL associated with pelvic and acetabular fractures and open debridement with incision placed close to the middle of the degloved area was the preferred method. They also reported that primary closure was associated with higher incidence of complications, including wound breakdown and infection. Application of MRI has been shown to be useful in identifying the MLL with capsule that would need to be treated with surgical debridement and keeping the wound open (Mellado J.M et al, 2005) Smaller lesions have been showed to be amenable to percutaneous drainage and compression (Tsur A. et al, 2006).
Harmet A. et al (2004) reported four cases of MLL with 2 patients treated with elastic bandages or corsets without surgical intervention and 1 patient who had compressive bandages applied after successful percutaneous drainage. The authors attributed to success of the compression therapy to small size of the MLL and appearance of healthy skin over the lesion.
The early recognition and treatment of MLL is more important in cases when the surgery is planned for fixation of pelvic or femoral fractures. The placement of external fixating pins through unrecognized MLL can lead to significant infectious complications. According to Hak D.J. (1997) the contents of the MLL were culture positive in 46%. In their series all patients with MLL were treated with incision and debridement before or during the surgery for pelvic or acetabular fractures. Tseng S. et al (2006) reported that early percutaneous drainage with débridement, irrigation, and suction drainage for the treatment of Morel-Lavallee lesions appears to be safe and effective. Fifteen of the nineteen patients had surgery for an associated pelvic or acetabular fracture. Seven of the nine patients in whom a pelvic fracture was treated surgically had percutaneous fixation of the posterior part of the pelvic ring as well as treatment of the Morel-Lavallee lesion during the same operative setting. Fixation of the remaining two pelvic fractures and the six acetabular fractures was deferred until at least twenty-four hours after the drain was removed.
This paper describes the case of MLL and provides the review of recent data on diagnosis, management and outcome of MLL.
CASE REPORT.
A 34 years old young man was transferred to our level 1 trauma center from other institution to where he was brought after being run over by bus. Due to low GCS score in the field he was intubated and transferred to that nearest hospital where he continued to be hypotensive requiring transfusion of 4 units of PRBC and about 3 L of crystalloid fluids. Upon arrival to HMC he remained hemodynamically unstable with SBP in 70s and dropping in hematocrit. His CT images from OSH were negative for intraabdominal injuries and he was taken to IR suite where he had pelvic angiogram, gelfoam embolization of left internal iliac artery, coil embolization of branch of right internal iliac artery posterior division and branch of inferior gluteal artery.
His complete work up and review of images showed complex pelvic ring injury with right sacral fracture, symphysis pubis disruption and right pubis fracture. In addition to orthopedic injuries, patient was found to have laceration of the skin from the anus to the dentate line and urethral injury. After stabilization he was taken to operating room for percutaneous fixation of right sacral fracture, open reduction and internal fixation of right pubis fracture, open reduction and internal fixation of symphysis pubis, removal of traction pin of right lower extremity placed at other institution. After the surgery he was taken to ICU for further resuscitation and initial care.
During the subsequent days, he was noted to have increased pain and ecchymoses over the left buttock and thigh. After further evaluation, it was suspected that he had a Morel-Lavallee lesion in this area.
On hospital day 5 he was taken to OR for irrigation and excisional debridement of left degloving deep hematoma and irrigation and excisional debridement of left deep thigh hematoma with degloving injury. Upon making the incision, a large hematoma with necrotic fat expressed itself from the proximal aspect of the wound and 1.2 L of hematoma was evacuated and necrotic fat was debrided and evacuated. The skin and subcutaneous tissue overlying the degloved area was not excised. The area of debridement was roughly 45 cm x 50 cm x 35 cm. Given the extend of necrotic process to the deep fascia, the fat and fascia were debrided and then 12 L of irrigation with normal saline was used to copiously wash out this wound.
Prior to thorough debridement, cultures were sent and antibiotics were administered. His gram stain and cultures from tissue samples taken in OR showed mixed gram positive flora which then helped to narrow down the antibiotic coverage.
After the debridement, three large number 10 drains were placed in the wound. During subsequent hospital stay two of the drains were removed and one drain was left in place. He was discharged home to family care and presented to the hospital two weeks later and taken to OR for complex irrigation and excisional debridement of left buttock necrotic skin and tissue measuring 25 x 20 cm. A knife was used to peel off the necrotic skin, fat and partial excision of fascia and gluteus maximus muscle. A curette was used to debride to healthy bleeding fascia and muscle. Three liters of irrigation with normal saline was used to irrigate this large wound. Then a large wound VAC was placed over the open wound area. During the same hospitalization he was then taken to OR on three more occasions for further irrigation and debridement of the open wound and wound VAC change. And finally he was then taken to OR by plastic surgery for surgical preparation of recipient site by debridement (400 square cm), left hip and buttock region and split-thickness skin grafting from left thigh to left hip and buttock region (400 square cm). Wound VAC was then used to pack the deep portion of wound posteriorly to maximize surface contact with the skin graft. Wound VAC was placed to 125 mm Hg of suction.
Postoperatively he continued to have wound VAC, which was subsequently removed and the recipient site as well as donor site for STSG were observed to be healing well.
After discharge from the hospital he had 2 month follow up with orthopedic and plastic surgery services and his left hip and buttock wounds has healed.
DISCUSSION.
The case described above well illustrates the need for early recognition and aggressive surgical treatment of the large MLL associated with the complex pelvic fractures. The attention to the initial stabilization of patient and treatment of life threatening injuries, often leads to delayed recognition of the MLL that can be a cause of significant morbidity and prolong hospital stay. This case also describes the need for team approach to the management of large MLL with the involvement of orthopedic and plastic surgeons as often these patients need reconstruction of the soft tissue defects with myocutaneous flap or STSG.
The combination of initial less aggressive approach with small incisions and percutaneous drainage with compressive dressing have been advocated in the treatment of MLL with varied success rates. However, in our case of large MLL with severe disruption of blood supply to the large area of separated skin and subcutaneous tissue, was likely a leading cause of failure with this less aggressive approach. More aggressive excision and debridement of the necrotic and semi-viable skin and subcutaneous tissue deemed only available option in this patient.

